Glucose, often referred to as blood sugar, is the primary source of energy for your body. It’s a simple sugar (monosaccharide) that circulates in your bloodstream, fueling everything from your brain to your muscles. While essential for life, maintaining balanced glucose levels is crucial for overall health. This article explores the ins and outs of glucose, how it works in your body, how to test and monitor it, and effective strategies for managing your blood sugar.
Table of Contents
The Role of Glucose in the Body
When you consume carbohydrates, your digestive system breaks them down into glucose. This glucose is then absorbed into the bloodstream. The pancreas, a vital organ, plays a pivotal role in this process by releasing insulin. Insulin acts as a key, unlocking your cells to allow glucose to enter and be used for energy.
- Energy Production: Glucose is the body’s preferred energy source. It powers everything from cellular functions to physical activity.
- Brain Function: The brain relies heavily on glucose for optimal performance. Fluctuations in blood sugar can affect concentration, mood, and cognitive abilities.
- Muscle Function: During physical activity, muscles use glucose for energy. Maintaining stable glucose levels is essential for sustained performance.
- Storage: Excess glucose is stored as glycogen in the liver and muscles. When needed, glycogen can be converted back into glucose to maintain stable blood sugar levels.
The Importance of Insulin
Insulin is a hormone produced by the beta cells of the pancreas. Its primary function is to regulate blood glucose levels.
- Facilitating Glucose Uptake: Insulin binds to receptors on cell membranes, signaling them to absorb glucose from the bloodstream.
- Regulating Liver Glucose Production: Insulin suppresses the liver’s production of glucose, preventing excessive release into the bloodstream.
- Promoting Glycogen Storage: Insulin stimulates the storage of glucose as glycogen in the liver and muscles.
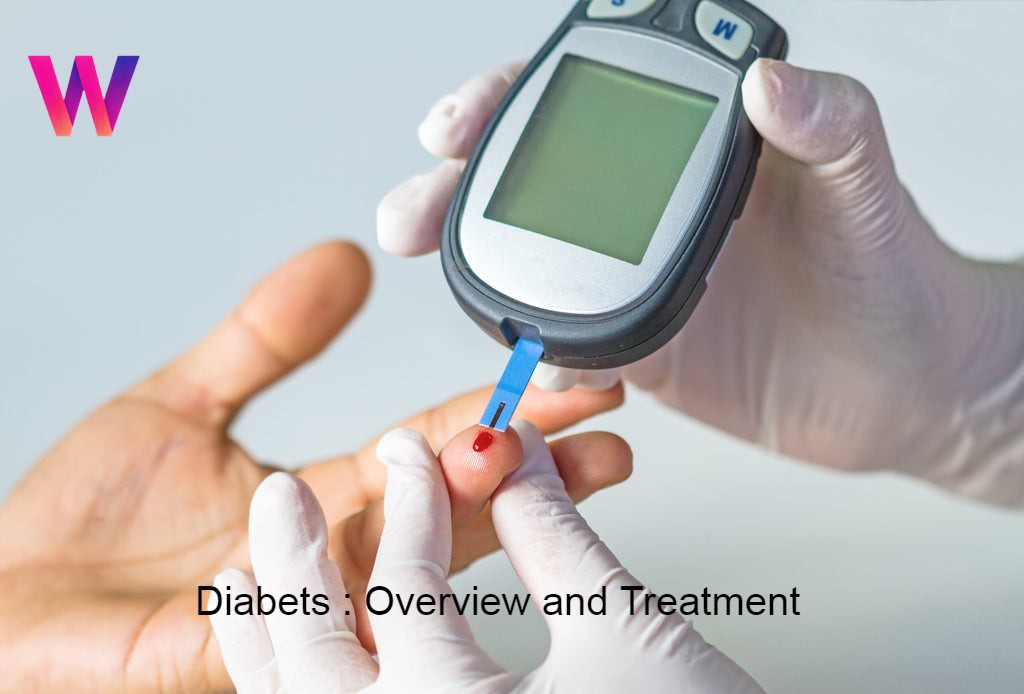
Testing and Monitoring Glucose Levels
Regular monitoring of glucose levels is crucial, especially for individuals with diabetes or those at risk.
- Blood Glucose Meters: These portable devices measure the amount of glucose in a small blood sample obtained from a finger prick. They provide instant readings, allowing for real-time monitoring.
- Continuous Glucose Monitoring (CGM) Systems: CGMs use a sensor inserted under the skin to measure glucose levels in interstitial fluid continuously. They provide real-time data and trend graphs, offering a comprehensive view of glucose patterns.
- A1C Test: This blood test measures your average blood glucose level over the past 2-3 months. It provides a long-term view of glucose control and is used to diagnose and manage diabetes.
- Oral Glucose Tolerance Test (OGTT): This test involves fasting overnight, drinking a sugary solution, and having blood glucose levels measured at specific intervals. It’s used to diagnose gestational diabetes and prediabetes.
Understanding Glucose Levels
- Normal Range: A fasting blood glucose level of 70-99 mg/dL is considered normal. Post-meal glucose levels should remain below 140 mg/dL two hours after eating.
- Hypoglycemia (Low Blood Sugar): Occurs when blood glucose levels drop below 70 mg/dL. Symptoms include sweating, shakiness, dizziness, and confusion.
- Hyperglycemia (High Blood Sugar): Occurs when blood glucose levels are consistently elevated. Symptoms include increased thirst, frequent urination, blurred vision, and fatigue.
Factors Affecting Glucose Levels
Several factors can influence glucose levels:
- Diet: Consuming high-carbohydrate foods, especially refined carbohydrates and sugary drinks, can cause rapid spikes in blood sugar.
- Physical Activity: Exercise helps improve insulin sensitivity and lowers blood glucose levels. However, intense exercise can sometimes cause a temporary rise in blood sugar.
- Stress: Stress hormones, such as cortisol and adrenaline, can raise blood glucose levels.
- Illness: Infections and illnesses can trigger hormonal changes that affect glucose metabolism.
- Medications: Certain medications, such as steroids, can raise blood glucose levels.
- Hormonal Changes: Fluctuations in hormone levels, such as during menstruation or pregnancy, can affect glucose control.
- Dehydration: When dehydrated the concentration of glucose in the blood can rise.
Complications of Poor Glucose Management
Uncontrolled high blood sugar can lead to serious health complications:
- Cardiovascular Disease: High blood sugar damages blood vessels, increasing the risk of heart disease, stroke, and peripheral artery disease.
- Neuropathy: Nerve damage caused by high blood sugar can lead to numbness, tingling, and pain in the extremities.
- Nephropathy: Kidney damage caused by high blood sugar can lead to kidney failure.
- Retinopathy: Damage to the blood vessels in the retina can lead to vision loss and blindness.
- Diabetic Ketoacidosis (DKA): A life-threatening condition caused by severe hyperglycemia, characterized by the production of ketones.
Strategies for Managing Glucose Levels
Effective glucose management involves a combination of lifestyle modifications and medical interventions:
- Balanced Diet: Focus on whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables. Limit refined carbohydrates and sugary drinks.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Weight Management: Maintaining a healthy weight can improve insulin sensitivity and glucose control.
- Stress Management: Practice stress-reducing techniques, such as meditation, yoga, or deep breathing exercises.
- Medications: Your doctor may prescribe medications, such as insulin or oral hypoglycemic agents, to help manage your blood sugar.
- Regular Monitoring: Consistent monitoring of glucose levels is essential for effective management.
- Hydration: Drinking enough water is very important.
- Sleep: Getting enough sleep helps regulate hormomes that influence glucose.
The Importance of Professional Guidance
Managing glucose levels effectively requires a personalized approach. Consult with a healthcare professional, such as an endocrinologist or certified diabetes educator, to develop a comprehensive management plan. They can provide guidance on diet, exercise, medication, and monitoring.
Conclusion
Glucose is essential for energy, but maintaining balanced levels is crucial for overall health. By understanding how glucose works in the body, monitoring your levels, and adopting healthy lifestyle habits, you can effectively manage your blood sugar and reduce the risk of complications. Regular consultations with healthcare professionals are vital for personalized guidance and support.