Kidneys quietly work day and night to keep your body in balance. They filter waste, regulate fluids, control electrolytes, and help with hormone production. When they begin to fail—slowly or suddenly—you may not notice right away. But early detection can make a huge difference in management and quality of life.
In this post, we’ll dig into what kidney failure really means, how it often begins, what early warning signs to watch for, who’s most at risk, how it’s diagnosed, and what steps you can take if you suspect something is wrong.
Table of Contents
What Is Kidney Failure?
Kidney failure (also known as renal failure) refers to a condition in which the kidneys lose their ability to filter wastes and excess fluids from the blood effectively. There are two major types:
- Acute kidney failure (acute kidney injury, AKI): Kidney function declines rapidly—over hours to days. It may be reversible with prompt treatment.
- Chronic kidney disease (CKD): Damage accumulates gradually over months or years. Often, early CKD has no noticeable symptoms.
As kidney function diminishes, waste products (like urea, creatinine), excess fluid, and imbalances in salts and minerals build up in the body—leading to many kinds of trouble. Knowing early signs gives you a chance to intervene and slow the progression.
Why Early Detection Matters
- The kidneys have a high reserve capacity. You can lose a lot of function before symptoms become severe. This means damage can progress while being silent.
- Early identification allows lifestyle changes, medicine, and close monitoring to slow decline.
- Delay in diagnosis could lead to complications: fluid overload, electrolyte imbalances, heart problems, bone issues, anemia, etc
Who’s at Higher Risk
Understanding risk factors helps you know when you should be more alert or ask for screening. Some key risk factors include:
- Diabetes (especially if blood sugar is poorly controlled) is a leading cause of CKD.
- High blood pressure (hypertension), which damages small blood vessels in the kidneys.
- Family history of kidney disease.
- Older age. Kidney function tends to decline with age.
- Certain medical conditions: autoimmune diseases, kidney infections, kidney stones, obstructive urinary tract issues, certain medications, etc.
- Lifestyle factors: obesity, smoking, high salt intake, dehydration, repeated use of nephrotoxic drugs (NSAIDs, etc.).
If you have one or more of these, routine checks (blood tests, urine tests, blood pressure monitoring) are wise.
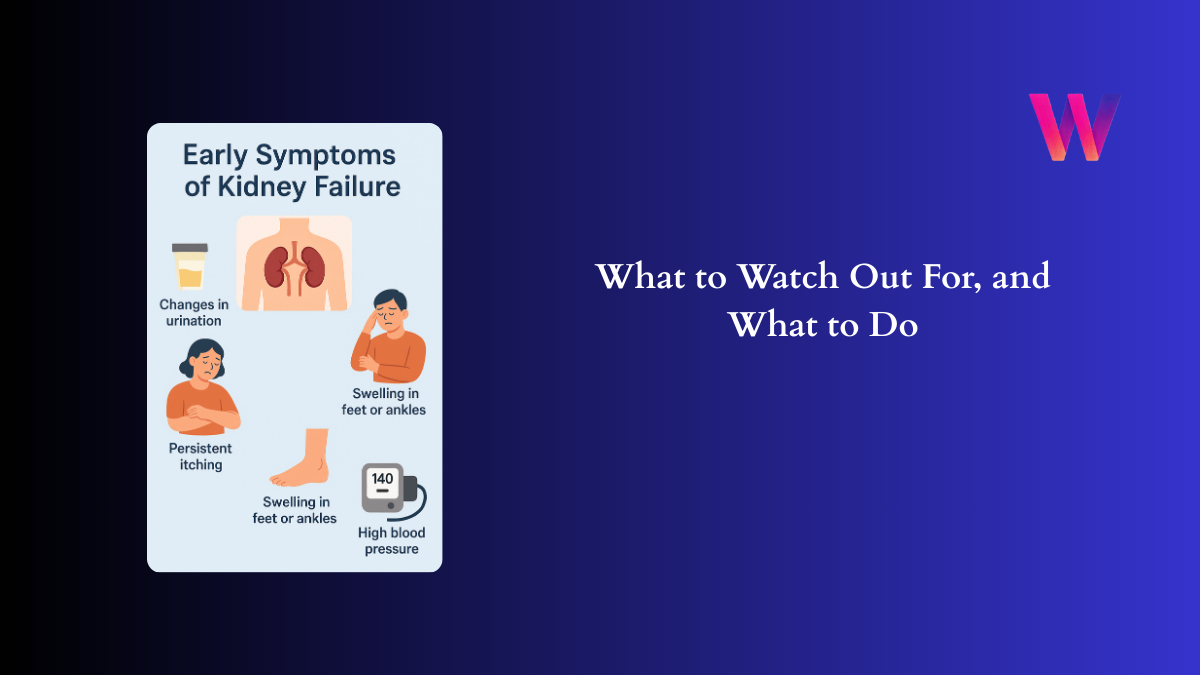
Early Symptoms of Kidney Failure (Subtle Signs)
These are signs that may appear in earlier stages of kidney dysfunction. They can be subtle, intermittent, or attributed to other causes—but put them all together and you have reasons to watch closely.
| Symptom | What it might indicate in terms of kidney function / physiology |
|---|---|
| Changes in urination | This includes urinating more often (especially at night), urinating less, dark urine, pale urine, foamy urine (suggests protein loss), or blood in urine. Damaged filters allow things like protein or red blood cells to leak through. |
| Fatigue and feeling weak | Waste buildup (like urea) and anemia (because damaged kidneys make less erythropoietin, which signals bone marrow to make red blood cells) reduce oxygen transport, causing tiredness. Even small efforts feel draining. |
| Loss of appetite / nausea / metallic taste | Waste products in blood can affect digestion and sense of taste. |
| Swelling (edema) in feet, ankles, legs, sometimes hands or face | Kidneys failing to balance fluid → retention of water and salt → swelling. |
| High blood pressure that’s hard to control | One both a cause and effect. Damaged kidneys can’t regulate fluid and salt well, affecting blood pressure; high blood pressure further damages kidney blood vessels. |
| Persistent itching / dry skin | Accumulation of wastes like urea, mineral imbalances (calcium, phosphorus) irritate skin. |
| Muscle cramps | Electrolyte disturbances (low calcium, high phosphorus, abnormal potassium) can trigger cramps. |
| Difficulty concentrating / “brain fog” | Toxin buildup, anemia, poor sleep, electrolyte shifts all affect cognition. |
| Sleep disturbances / restless legs | Metabolic alterations and accumulation of waste can make sleep uneasy. Also fluid overload or breathing trouble may contribute. |
| Shortness of breath | If fluid builds up (in lungs) or anemia is severe enough, breathing becomes harder. |
| Changes in weight / swelling of face | Due to fluid retention. Sometimes sudden weight gain. |
How Early Is Early? Stage 1 & Stage 2 CKD
Kidney disease is divided into stages. Early stages (Stage 1 and Stage 2) often show few or no symptoms, or very mild ones. Knowing what tends to occur in these stages helps:
- Stage 1: Kidneys are working nearly normally (eGFR ≥ 90), but there are signs of damage—protein in urine (albuminuria), structural changes seen via imaging. Often no or very mild symptoms.
- Stage 2: Slight decline in kidney function (eGFR 60-89), mild damage. Symptoms still often subtle. Small changes in urine, perhaps slight swelling or higher blood pressure.
Because symptoms are mild or non-specific, many people don’t realize something is wrong until Stage 3 or 4.
Differences Between Acute and Chronic Early Symptoms
| Feature | Acute Kidney Failure | Early Chronic Kidney Disease |
|---|---|---|
| Onset | Rapid (hours to days) | Slow (months to years) |
| Urine output | Often decreases sharply (oliguria) or stops | May change gradually, increase/decrease, foamy or discoloured urine |
| Symptoms intensity | More severe quickly: nausea, confusion, fluid overload, possible electrolyte crisis | Milder, often vague: fatigue, mild swelling, early hypertension |
| Reversibility | Often reversible if cause treated early | Damage tends to accumulate; reversible only in early phase; progression often slowed rather than reversed |
Why Symptoms Are Often Missed or Misattributed
- Early symptoms are vague (“just tired”, “my back hurts”) and often blamed on stress, aging, dehydration.
- People with risk factors (diabetes, high BP) may already have some symptoms but think they are part of those conditions.
- Slow progression means body adapts, so the sense of “normal” shifts.
- Lack of routine screening: many people don’t get urine tests or kidney function tests unless there’s a reason.
When You Should See a Doctor
If you notice any of the following, especially in combination or over a period of time, schedule a check-up. Early action is key.
- Persistent changes in urination: volume, color, foam, blood
- Unexplained fatigue or weakness
- Swelling of ankles, feet, face
- Poor appetite, nausea, or metallic taste
- Persistent high blood pressure that’s hard to control
- Skin irritation, itching without obvious cause
- Muscle cramps that are recurring
- Difficulty concentrating, memory problems or “brain fog”
If you have known risk factors (diabetes, hypertension, family history, certain medications), even mild symptoms merit investigation.
How Kidney Function Is Diagnosed
When you see a doctor, here are the main tools used to assess kidney health:
- Blood tests
- Creatinine and blood urea nitrogen (BUN) to see waste level.
- Estimated glomerular filtration rate (eGFR) to measure how well kidneys are filtering.
- Electrolytes (potassium, sodium, phosphorus, calcium).
- Urine tests
- Check for protein (albuminuria/proteinuria).
- Blood in urine (hematuria).
- Microscopy, sometimes microalbumin tests.
- Imaging
- Ultrasound, CT or MRI to look for structural issues (kidney size, blockages, cysts).
- Other assessments
- Blood pressure monitoring
- Checking for anemia (hemoglobin levels)
- Assessing lifestyle, medications, other health conditions
- Monitoring over time
- Because kidney disease often progresses slowly, multiple tests over months can reveal trends.
What to Do If Early Signs Are Present
If diagnostic tests suggest early kidney damage, there’s a lot you can do to slow progression, relieve symptoms, and protect what kidney function you still have.
- Manage underlying conditions
- Tight control of blood sugar (for diabetics).
- Control blood pressure. Certain medications (ACE inhibitors, ARBs) protect kidneys.
- Treat urinary tract infections, avoid obstructions.
- Dietary adjustments
- Reduce salt intake.
- Moderate protein intake—enough to maintain health but not overload kidneys.
- Stay hydrated—but avoid overhydration if kidney output is very low.
- Avoid high-phosphorus and high-potassium foods if laboratory values indicate they are problematic.
- Lifestyle changes
- Maintain healthy weight.
- Exercise regularly.
- Stop smoking.
- Limit use of over-the-counter pain killers (especially NSAIDs) which can strain kidneys.
- Regular monitoring and specialist care
- Periodic blood and urine tests to track kidney function.
- Involve a nephrologist if things indicate worsening function.
- Screening for cardiovascular complications (kidney disease raises risk).
- Medications
- As advised by a physician: e.g. to manage blood pressure, cholesterol, acid/base imbalances, anemia.
Common Myths & Misconceptions
- “If I feel fine, my kidneys are fine.” Not necessarily—kidneys can lose function without overt symptoms.
- “Only older people get kidney disease.” Younger people can too—especially with risk factors.
- “Brown-coloured urine always means dehydration.” It could, but blood in urine is a red flag. Don’t ignore.
- “Protein in diet is always bad for kidneys.” Protein is essential; the key is moderation and balance, especially if kidney damage is already present.
What That Means for You (Takeaways)
Here are practical steps you can start today, or advise your readers to take, to catch kidney issues early or avoid them altogether:
- Know your risk factors: family history, chronic disease, etc.
- Get basic screening: eGFR, urine protein, blood pressure check. If you have risk factors, ask your doctor to do this annually or per their guidance.
- Observe your body: changes in urination, fatigue, swelling, skin changes. Don’t dismiss mild but persistent symptoms.
- Keep a notebook or health app to record symptoms over weeks/months: “How many times I urinate at night”, “Any swelling in ankles”, etc. Patterns help.
- Adopt kidney-friendly habits early even before diagnosis: balanced diet, hydration, physical activity, avoid smoking.
Conclusion:
- Kidney failure often begins quietly; symptoms may be vague and easily dismissed.
- Early symptoms include changes in urination, fatigue, swelling, appetite loss, itchiness, muscle cramps, cognitive issues, among others.
- Risk factors like high blood pressure, diabetes, family history, age increase the odds.
- Diagnosis involves blood and urine tests, imaging, regular monitoring.
- Early detection and lifestyle / medical interventions can greatly slow progression, reduce complications, and preserve quality of life.